What Is Atherosclerosis?
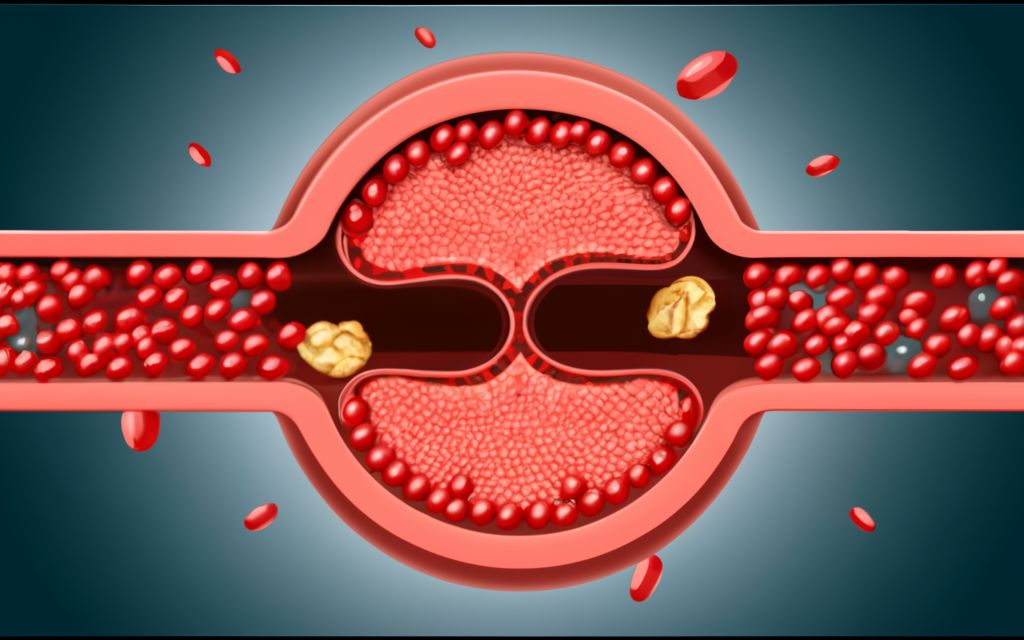
Imagine your arteries, the vital highways transporting life-giving blood throughout your body, becoming clogged and narrowed. That’s the essence of atherosclerosis, a chronic progressive disease characterized by the buildup of plaque (made up of cholesterol, fat, calcium, and cellular debris) inside the artery walls. This buildup restricts blood flow, eventually leading to serious complications like heart attack, stroke, and even limb amputation.
Symptoms:
Atherosclerosis often progresses silently, with symptoms only manifesting when blood flow becomes significantly restricted. However, some subtle signs might emerge:
- Chest pain (angina): Discomfort or chest tightness, especially during exertion, indicating reduced blood flow to the heart.
- Pain in the legs or arms: Reduced blood flow to limbs can cause pain, particularly when walking or exercising.
- Numbness or weakness in limbs: Decreased circulation can lead to limb numbness or weakness.
- Erectile dysfunction: Reduced blood flow to the penis can affect erectile function in men.
| Stage of Atherosclerosis | Description |
|---|---|
| Stage 1: Initiation | In this stage, injury or damage occurs to the inner layer of the artery, known as the endothelium. This damage can result from factors such as high blood pressure, smoking, or high cholesterol levels. |
| Stage 2: Fatty Streaks | Fatty streaks begin to form as cholesterol and other fats accumulate within the damaged area of the artery wall. These streaks are considered the earliest visible sign of atherosclerosis. |
| Stage 3: Plaque Formation | Over time, the fatty streaks can evolve into plaques, which are made up of cholesterol, calcium, cellular waste, and other substances. Plaques can protrude into the arterial lumen, narrowing the vessel and restricting blood flow. |
| Stage 4: Progression | In this stage, the plaques continue to grow and may harden, leading to further narrowing of the arteries. The progression of atherosclerosis can increase the risk of complications such as heart attack or stroke. |
| Stage 5: Complications | Complications of atherosclerosis may include the formation of blood clots within narrowed arteries, which can obstruct blood flow to vital organs and tissues. These complications can result in serious cardiovascular events. |
Complications:
Untreated atherosclerosis sets the stage for potentially life-threatening complications:
- Heart attack: When a plaque ruptures and blocks blood flow to the heart, a portion of the heart muscle dies, leading to a heart attack.
- Stroke: If a plaque ruptures and blocks blood flow to the brain, it can cause a stroke, damaging brain tissue and impacting function.
- Peripheral artery disease (PAD): Atherosclerosis in the arteries supplying blood to limbs can lead to PAD, causing pain, numbness, and even tissue death in extreme cases.
- Aortic aneurysm: Weakened artery walls due to atherosclerosis can form an aneurysm (bulge) in the aorta, the main artery carrying blood from the heart, which can rupture and be life-threatening.
Medicines:
Several medications play crucial roles in managing atherosclerosis:
- Statins: Lower “bad” cholesterol (LDL) and raise “good” cholesterol (HDL).
- Angiotensin-converting enzyme (ACE) inhibitors or angiotensin-receptor blockers (ARBs): Lower blood pressure and protect the heart.
- Antiplatelet medications: Reduce blood clot formation, preventing blockage in narrowed arteries.
- Vasodilators: Widen blood vessels to improve blood flow.
Coronary Angioplasty:
When medication isn’t sufficient, minimally invasive procedures like coronary angioplasty might be employed:
- Balloon angioplasty: A tiny balloon is inserted into the narrowed artery and inflated to open it.
- Stent placement: A small mesh tube is placed inside the artery to keep it open after ballooning.
What is the main cause of arteriosclerosis?
While the exact cause of atherosclerosis is unknown, several factors contribute:
- High cholesterol: Elevated levels of LDL cholesterol significantly increase the risk.
- High blood pressure: Puts additional strain on arteries, accelerating plaque buildup.
- Smoking: Damages blood vessel walls and promotes inflammation, furthering plaque formation.
- Diabetes: Uncontrolled blood sugar levels contribute to inflammation and damage blood vessels.
- Obesity: Excess weight strain the heart and blood vessels, promoting atherosclerosis.
- Family history: Having a family history of heart disease increases your risk.
- Inactive lifestyle: Lack of physical activity contributes to higher cholesterol and blood pressure.
What are the warning signs of atherosclerosis?
As mentioned earlier, atherosclerosis often progresses silently. However, paying attention to certain risk factors and adopting a proactive approach are crucial:
- Age: Risk increases with age, especially over 45 for men and 55 for women.
- Symptoms: Be aware of chest pain, leg pain, or unusual limb sensations.
- Family history: Knowing your family’s heart health history is essential.
- Lifestyle: Monitor your cholesterol, blood pressure, and weight and address any concerns.
What is the best treatment for atherosclerosis?
The best treatment is a multi-pronged approach incorporating:
- Lifestyle changes: Quit smoking, adopt a healthy diet low in saturated fats and high in fruits and vegetables, maintain a healthy weight, and engage in regular physical activity.
- Medications: Take prescribed medications like statins, blood pressure medications, and antiplatelet agents as directed by your doctor.
- Procedures: If necessary, consider minimally invasive procedures like angioplasty and stenting to open blocked arteries.